Lameness & The Lameness Exam: What Horse Owners Should Know

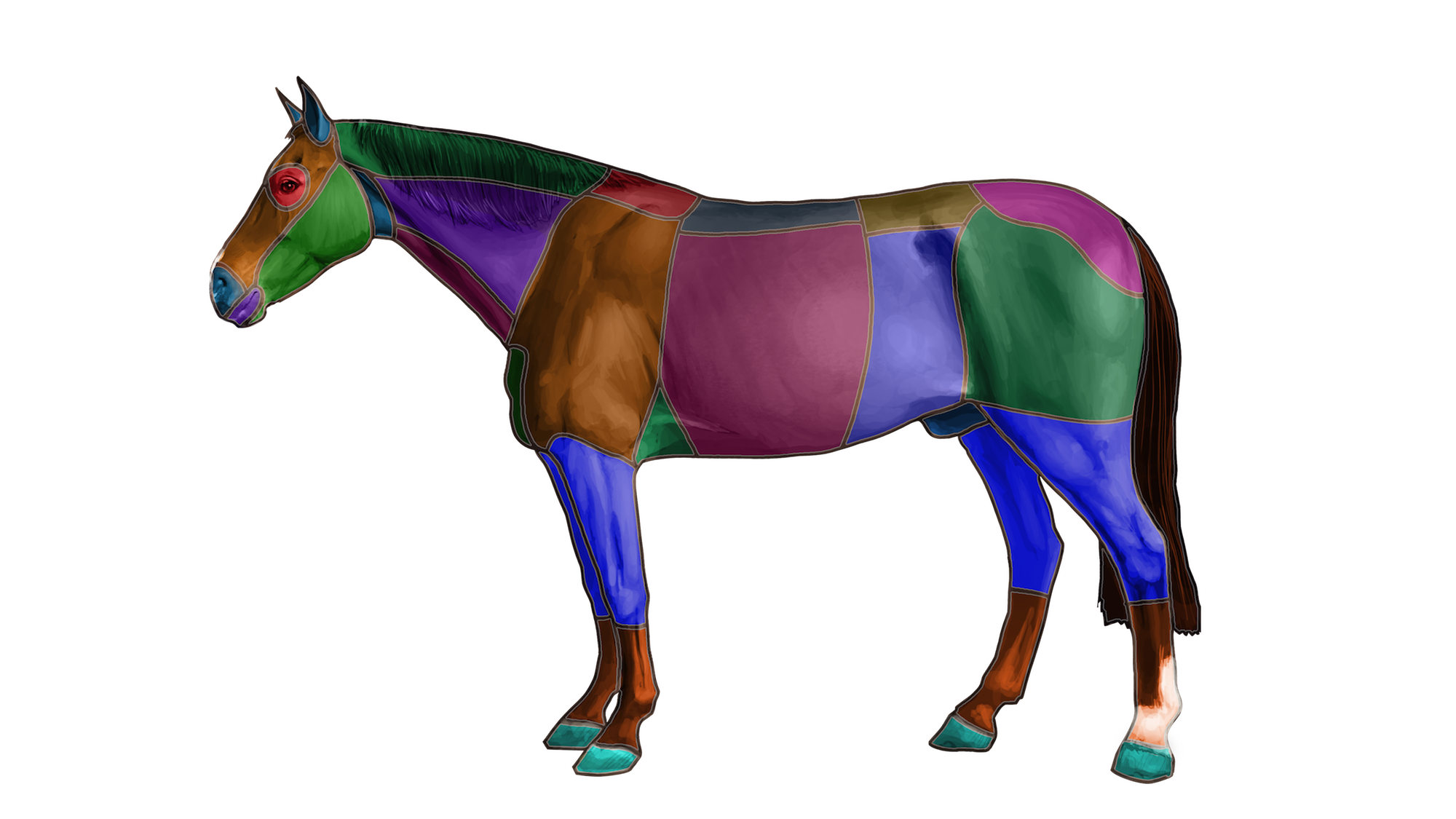
WHAT IS EQUINE LAMENESS?
Lameness is a term used to describe a horse’s change in gait, usually in response to pain somewhere in a limb, but also possibly as a result of a mechanical restriction on movement. We all think of lameness when a horse is obviously limping, but lameness may only cause a subtle change in gait, or even just a decreased ability or willingness to perform.
A horse can become lame from a variety of causes (conditions or ailments), involving almost any anatomic region within a limb. Some conditions are more easily diagnosed and treated than others.
For equine veterinarians, lameness diagnosis and treatment is both science and art. It requires a solid understanding of equine anatomy and physiology, conformation, biomechanics, and medicine, and yet it requires adaptation in response to changing conditions, horse types, uses and personalities, and owner needs.
Lameness accounts for the greatest losses for the equine industry – hundreds of millions of dollars annually. Lameness affects individual horses of all kinds and all levels, from subtle, reduced performance to loss of use, to chronic severe pain resulting in euthanasia. Sadly, many horses are asked to perform when they are in pain because of riders’ failure to recognize lameness.
There is a vast amount of erroneous lameness information on the Internet, along with reliable, useful information. As a horse owner, you are faced with a universe of well-advertised but completely unproven “miracle cure” products which claim to address every ailment. What is missing from the equation is a proper diagnosis, which only a trained and experienced veterinarian can provide.
To be the best caretaker, you should understand the basics of equine lameness. Here are 7 goals you should try to attain:
1. Increase your awareness of lameness in horses. It’s very common – usually right under your nose.
2. Increase your knowledge of basic equine anatomy, especially of the lower legs.
3. Know the most common lameness conditions that affect horses of YOUR breed, type, conformation, and discipline. Know the Observations that might suggest those conditions.
4. Recognize that worsening performance under saddle, or resistance to performance can hint at lameness. Just because YOU can’t detect lameness does not mean it does not exist. It can be very subtle. Apparent back soreness or stiffness can also relate to underlying lameness.
5. Understand something about the veterinary lameness exam itself, and its advantages and limitations.
6. Recognize the relationship between conformation (form), function and lameness. Recognize certain conformational attributes and how they predispose to lameness.
7. Know the factors that minimize lameness and musculoskeletal injury in your horses. The most important are conditioning and fitness, matching of conformation to use, hoof care and shoeing, and nutrition.
A basic understanding of lameness in horses is of great value and will assist you with:
• PURCHASE: Be able to roughly detect lameness and avoid horses that are lame. Understand the value of a pre-purchase exam, whereby an equine veterinarian assesses lameness and conformation issues, as well as the health of the whole horse, before purchase.
• MANAGEMENT & PREVENTION: Recognize conformational predispositions in your horses and manage or treat for the prevention or reduction of lameness.
• PERFORMANCE: Recognize, or at least consider when lameness may be the root cause of a horse’s poor performance (versus training or riding issues) so that lameness conditions can be promptly diagnosed and treated.
• BREEDING: Understanding basic equine form and function allows breeders to select horses that are of superior conformation and thus less likely to become lame.
ORIGINS OF LAMENESS
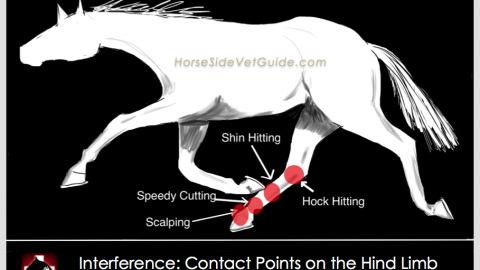
Lameness usually results from pain in an anatomic location within a limb, but can also result from mechanical restrictions on limb movement without pain. Visible gait deficits indistinguishable from painful conditions can result from a mechanical impediment to a horse’s movement. The classic example of this is fibrotic myopathy – scar tissue resulting from a tear of the hamstring muscle in the hindquarters. The scar shortens the hamstring muscle unit, and causes a characteristically abnormal gait, irrespective of pain.
Lameness results from pain coming from any part of a limb that contains nerve endings. Pain from skin wounds, connective tissue bruising, muscle pain, arthritis (joint inflammation), tendon sheath and bursal inflammation, tendon and ligament injury, and bone injury can all result in lameness that cannot be differentiated by observing the horse’s gait.
Certain breeds and disciplines are more commonly predisposed to developing specific lameness conditions. Examples include arthritis in the knee (carpus) in racehorses, hock arthritis in cutting horses, and hind limb suspensory lameness in dressage horses.
It’s important to know that the site and nature of the injury cannot necessarily be determined based on the appearance of the lameness or the way a horse moves.
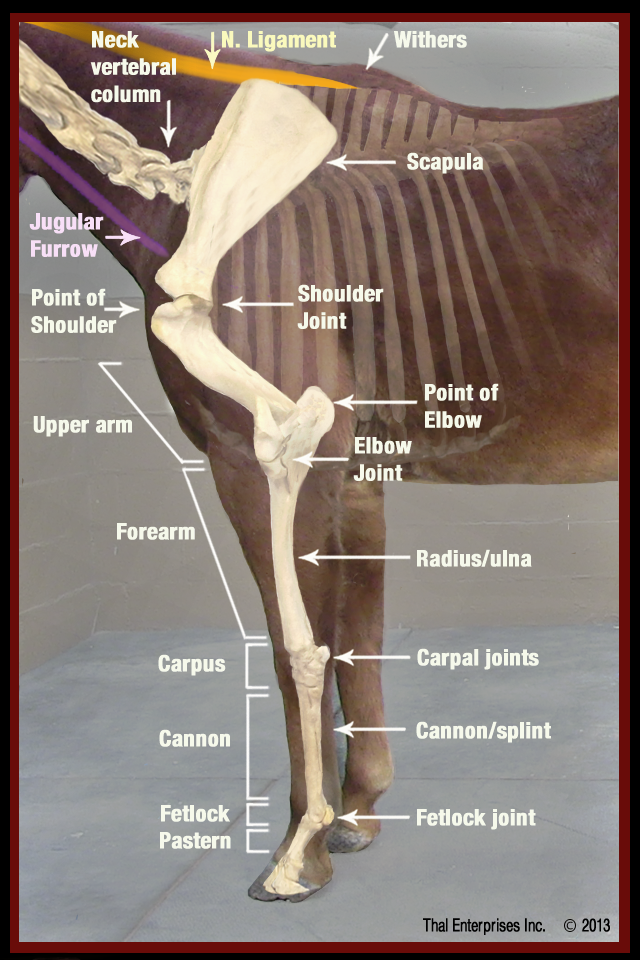
Some of the basic bones and landmarks of the equine front limb.
Forelimb lameness is easier for most people to recognize than hind limb lameness. The mechanics of the forelimb causes lameness to usually be more consistent in appearance and more obvious to the untrained eye.
Hind limb lameness is generally much more difficult to visualize and diagnose. This is especially true of subtle upper hind limb conditions. The massive musculature of the upper hind limb makes it much harder – even for an experienced examiner – to see and feel deeper structures, and more difficult to image these structures using radiographs and ultrasound.
A high percentage of lameness in the forelimb originates in the hoof. Upper forelimb lameness is not common in adult horses.
Conformation correlates directly with the mechanical function of the limb and particular conformation characteristics can predispose to particular lameness conditions. Horses with poor conformation are more likely to experience problems with feet, joints, tendons and ligaments than are horses of “normal”

Example of a “bench knee” – the cannon bone is set outward from the upper limb.
conformation. An example is “Bench Knee”, in which the cannon bone is set outward from the upper limb. This causes uneven mechanical loading of the carpus, predisposing to medial splint bone injury and carpal arthritis.
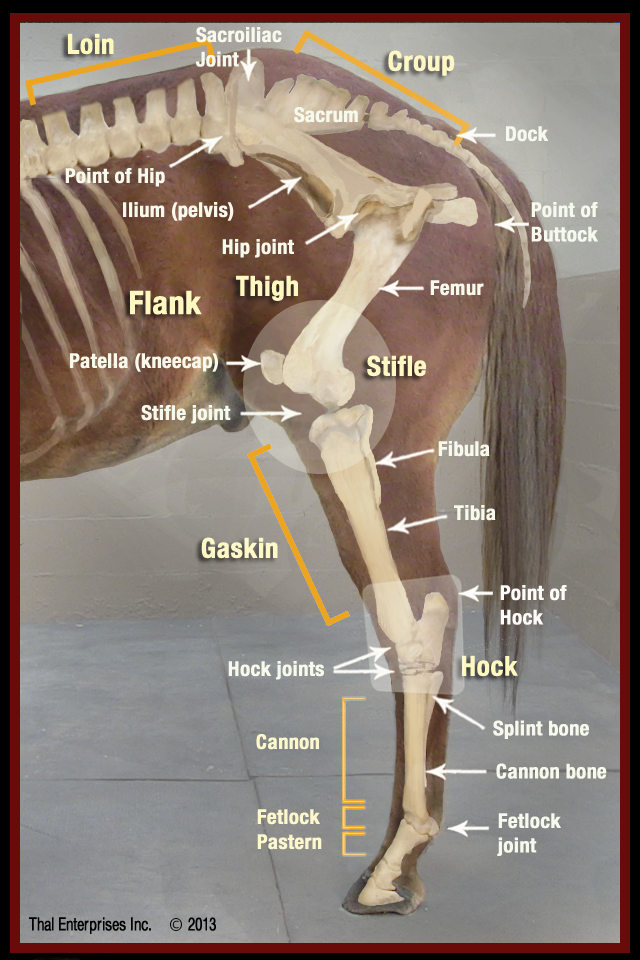
Some of the basic bones and landmarks of the equine hind limb.
THE LAMENESS EXAM
The lameness exam is a multi-step methodical veterinary exam wherein a veterinarian tries to determine where the pain in a limb originates and the nature of that pain. Only once a diagnosis is made can the best treatments be chosen.
Generally, lameness exams consist of (1) a careful history, (2) a standing exam (3) an exam in movement, (4) flexion and hoof tester exams, (5) diagnostic anesthesia – nerve and joint blocks, and (6) imaging the site of injury – radiographs, ultrasound, MRI and others. The diagnosis and treatment plan is derived from a synthesis of findings from all of the above parts of the lameness exam.
HISTORY: The first step in a lameness evaluation is a thorough history of both the horse and the injury. Information gathered about the horse includes breed, age, and prior use all of which provide clues to the problem. The history of the injury includes the date that lameness was first noticed, how severe the lameness has been, and how it occurred, if known. All of these are important questions that veterinarians ask, and you should try to be as complete as possible in your responses.
STANDING EXAM: A standing examination is done at a distance to evaluate the horse’s conformation and general appearance. This is followed by a more careful visual examination and palpation of specific anatomic structures for swelling, heat, and pain.
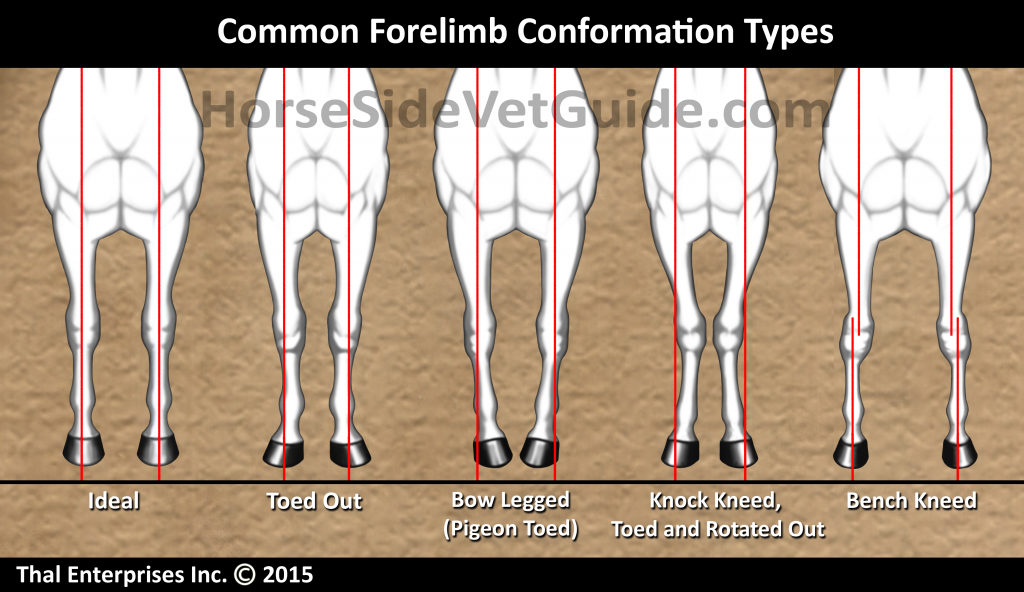
Common Equine Forelimb Conformation Types

The author free-lungeing and observing a trotting horse in the round pen.
EXAM IN MOVEMENT: The next part of the exam involves observation of the horse in movement. Lameness is mostly evaluated at the trot. Most thorough lameness exams are performed on firm to hard, consistent footing. Examination often includes trotting in hand in straight lines, and circles to both directions. It may also include moving a horse up or down inclines or through specific patterns. For the diagnosis of some types of lameness problems, having a rider up can be advantageous.

The author palpating the flexor tendons of a Quarter Horse.
FLEXION EXAMS: Flexion exams involve putting specific joints or regions of the limb under stress for a specified and consistent period of time. The horse’s degree of lameness is assessed before and after flexion. The result, which is the change in severity of lameness following flexion, provides additional information regarding the origin of the pain. As with many parts of the exam, flexion tests are subjective, and the vet must interpret them in light of what is considered normal for that specific horse.
HOOF TESTERS: Hoof testing involves the use of a pincer-like tool to put pressure on specific regions of the foot in search of a pain response. As with flexion exams, the key to accurate interpretation of hoof tester examination is knowledge of what constitutes a normal response. This can only be gained through a methodical approach, and lots of experience with different types of horses and hooves.

The author performing a hock/stifle flexion exam.
Once these things have been done, the veterinarian usually has determined which limb is lame, and may have an idea where the pain is located within that limb.
At this point, nerve blocks may then be necessary to determine precisely where the pain is located.
NERVE & JOINT BLOCKS: Nerve blocks are used to methodically numb portions of the limb as a means of finding the site of pain, using the process of elimination. Also known as diagnostic anesthesia, “blocking” is the injection of a local anesthetic agent around specific nerves or into specific joints or other structures. The horse is examined at the trot before the block, and the degree of lameness determined. Then the area in question is numbed, and the horse is asked again to trot off. Either there is improvement in the lameness or not.

The author has placed a needle alongside the palmar digital nerve and is preparing to inject local anesthetic to “block the nerve”. This will numb the heel and sole of the hoof.
If there is not, the process is continued on specific nerves progressing up the limb until the lameness is visibly lessened. Specific joints and tendon sheaths can also be blocked for a more specific localization of lameness. Blocks into a joint or tendon sheath require surgical cleanliness and technique to prevent infection of these structures. Limitations of blocking include spread of local anesthetics to adjacent regions, clouding the interpretation of the results.
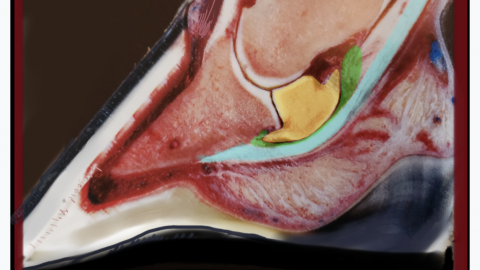
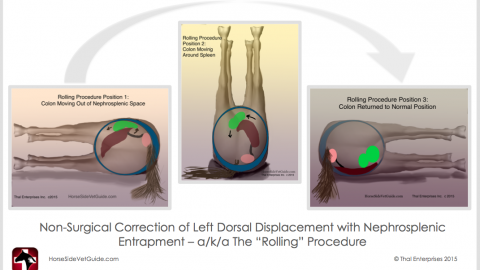
IMAGING THE SITE OF PAIN: Once the site of pain is located, diagnostic imaging is used to view the structures in the area and provides additional information about the nature of the injury. Diagnostic imaging includes radiography to image bone and ultrasound to image soft tissues, but may also include thermography, MRI, CT Scan and Nuclear Scintigraphy (bone scan).
Radiography is the main imaging diagnostic used to image bone. It is considered less useful for imaging of soft tissues, although it does provide some information. Radiographs are often performed in the field with portable equipment. More difficult studies on larger body parts are often better performed in a clinic setting. In the last decade, digital radiography has become the standard in equine vet practices. It produces high quality digital images on a screen within seconds. Examples of diagnoses that could be made via radiographic interpretation are chronic arthritis and fractures.
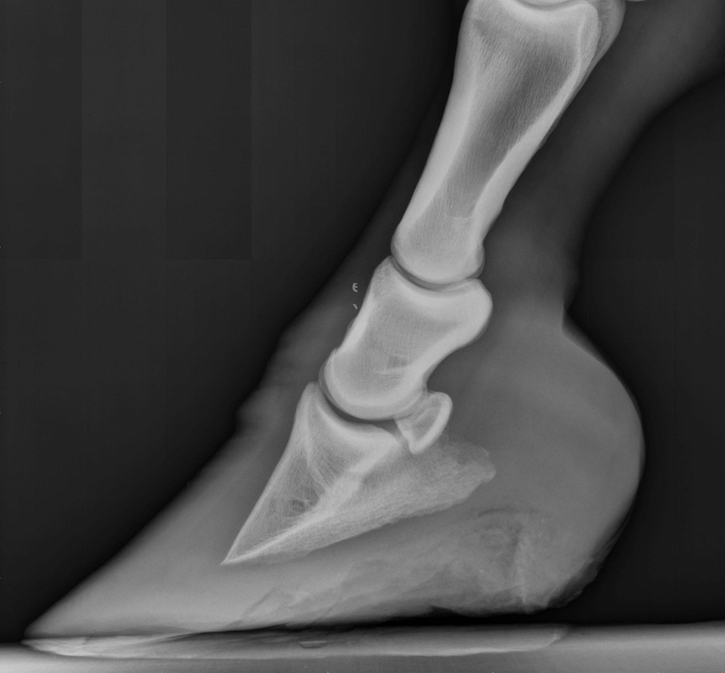
Radiograph – Laminitis, Mild Rotation
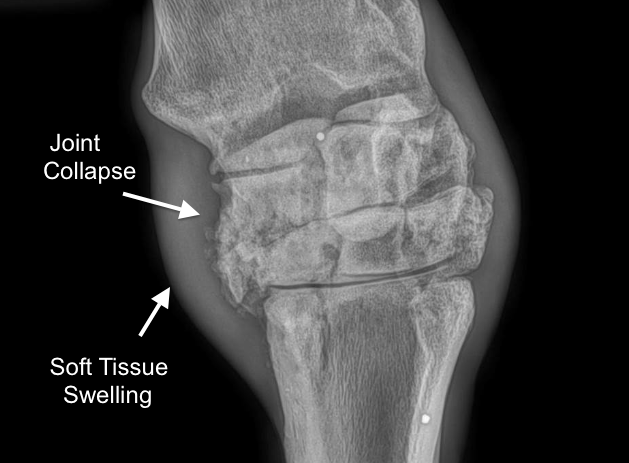
Severe Carpal Arthritis
Ultrasound utilizes sound waves traveling through tissues to image those tissues. It is excellent for imaging soft tissues, but cannot penetrate healthy bone. It is used commonly to image tendons, ligaments, the surfaces of bone, and other soft tissues. An example of a diagnosis that could be made via ultrasound is a tear or strain of a specific ligament or tendon.
Other, more advanced and expensive diagnostics such as MRI, Nuclear Scintigraphy (bone scan), and CT Scan are often reserved for more difficult to diagnose lameness cases or to provide additional information to the diagnosis. Arthroscopic surgical exploration is an important and commonly used diagnostic that allows direct visualization of the inside of joints.
See the related Topic: “Subtle or Hard to Diagnose Lameness: What Horse Owner’s Should Know” for a more detailed discussion of these advanced diagnostics.
LAMENESS TREATMENTS
All of the above steps, when performed properly and assembled and interpreted correctly, help to provide an accurate diagnosis and form the basis for a treatment program. Appropriate treatments will depend on the DIAGNOSIS. Ultimately, the treatment selected will depend on many factors, including your budget.
Examples of veterinary treatments used to address various lameness diagnoses include:
-
Joint (intra-articular) injections of steroids and other substances to reduce inflammation and pain in an arthritic joint.
-
Systemic (oral or injectable) anti-inflammatories and pain relievers to manage multiple pain sources, to manage chronic pain in older or debilitated horses, and as an adjunct to more specific therapies used.
-
Surgery, especially arthroscopy, is used to treat certain types of lameness. The most common is arthroscopic surgery, wherein repairs are made to the joint surface through several tiny incisions, and using a tiny camera and instruments inserted into the joint.
-
There are also a multitude of other newer therapies available including Pulsed Extra-Corporeal Shockwave, Stem Cell Injection, Injection of Platelet Rich Plasma, Autologous Conditioned Serum, IRAP and others. These are generally classed as “regenerative therapies” wherein the body is manipulated in some way to heal itself without externally derived medications. This is the exciting forefront of medicine and is the topic of another article.
-
Complementary therapies like acupuncture, chiropractic, massage and other treatments may have additional value in some cases but are not a substitute for a thorough lameness evaluation.
CONCLUSION
While lameness in horses cannot be prevented, it can be minimized through your understanding of the factors involved in its development.
Educate yourself, and work with your trusted equine veterinarian to diagnose problems early on. In this way, appropriate and effective treatments can be used, alleviating pain and slowing progression of problems, and enabling horses to get back to comfortable, sustainable work.
While new imaging techniques add a great deal to our understanding, a methodical clinical veterinary exam will always be the cornerstone of lameness diagnosis and should precede use of these diagnostics. While novel treatments are exciting, keep in mind that many of these treatments are in their infancy and are still unproven. It’s wise to consider the evidence for their effectiveness before using these costly therapies on your horses.
Most importantly, recognize the value of a veterinary diagnosis. Treatment without diagnosis can in some cases be a waste of money, time and resources.
By Doug Thal, DVM DABVP. Certified in Equine Vet Practice, Creator of Horse Side Vet Guide
Last Updated May 2016