Horses are predisposed to injure their eye, skull, and soft tissue structures of the head due to their living conditions, their curious and sometimes flighty behavior and the prominent location of the eyes on either side of their head. Below are examples of emergencies that would constitute immediate evaluation by your primary care veterinarian. Depending on the severity, your primary care veterinarian may refer your horse to an ACVS board-certified veterinary surgeon for further care:
- Laceration of the upper/lower eyelid
- Conditions affecting the cornea
- Corneal ulcer
- Melting corneal ulcer
- Corneal perforation and iris prolapse
- Corneal laceration
- Fracture of the orbit of the skull
- Foreign body underneath the eyelid, on the surface of the cornea, under the third eyelid or within the eye itself
- Change in orientation of eyelashes or squinting of eyelids: Normally the eyelashes point horizontally out to the side, but with eye pain, the eyelashes will start to point vertically down towards the ground and/or are held tightly closed (Figure 1).
- Eyelid or facial swelling: Fractures of the orbit may result in swelling of the eyelids, abnormal shape to the skull, air pockets under the skin that crackle when touched, bleeding from the nose and/or a bulging look to the eyeball. Fracture of the orbit may result in damage to the nerve that provides vision and cornea, resulting in corneal ulceration or blindness. If you are not sure, the other side of the head is useful for comparison (Figure 2).
- Increased amount of discharge from the eye (either clear or thick and butty) (Figure 3). You may also notice that more flies will congregate around the discharge.
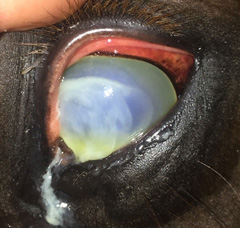
- Buttiness or discoloration of the cornea, may be red, white, blue (Figure 4 and 5), or yellow discoloration of a portion of or the entire cornea.
- The corneal may be white with an area that looks like its “melting” (Figure 6)
- Appearance of blood vessels on the cornea (Figure 7). The presence of blood vessels on the cornea is abnormal and is the eye’s healing response to a long standing problem to the cornea.
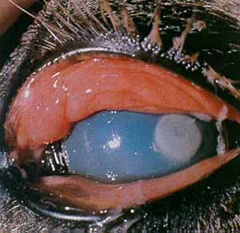
- Rupture (Corneal Perforation and Iris Prolapse): A full thickness hole in the cornea may be the result of traumatic injury to the eye or progression of a melting corneal ulcer. These require emergency surgical repair. When a full thickness hole develops in the cornea, the colored iris can protrude through the defect in the cornea, filling the hole with tissue (Figures 8a, 8b, and 9).
- Corneal laceration: May be either non-perforating (extending only part way through) or perforating (full thickness) and the result of either blunt or sharp trauma. Perforating (full thickness) corneal lacerations are surgical emergencies.
Foreign bodies (metal, plant material, etc): (metal, plant material, etc.): Can be found underneath the eyelids, on the surface of the cornea, under the third eyelid or within the eye itself. Most foreign bodies affect the cornea either by mechanical irritation, resulting in a painful corneal ulceration, or by puncturing the cornea.







Your veterinarian may recommend or perform some/all of the following procedures:
- Sedation to allow for local or regional nerve blocks or anesthetic agents applied directly to the surface of the eye and eyelid in order to allow examination.
- Examination of the eyelids, the cornea and deeper structures of the eye (iris, lens and, if possible, the retina) using specialized equipment.
- Evaluation of ulceration to the cornea using special stains such as fluorescein. Ulceration will result in a green fluorescence after application (Figure 10 and 11).
- Evaluation of tear film distribution using Rose-Bengal stain. This film is distributed over the corneal surface each time the eyelids close or blink. Disruption of the corneal tear film predisposes the eye to serious complications, including infection with fungal organisms and drying of the surface of the eye.
- Evaluation of tear film production using a Schirmer Tear test.
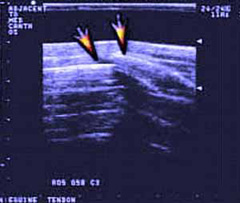
- Corneal scraping may be performed for cytology to look at the cells present (bacteria and/or fungal) and a swab may be submitted for culture and sensitivity to determine if an infection is present. Depending on the initial examination; radiographs (Figure 12) and/or ultrasound (Figure 13) may be performed by your veterinarian to identify fractures and abnormalities of the deeper structures of the skull/eye.



Prognosis for vision after an eye injury depends on the type and severity of the injury and whether adequate treatment can be provided.
- Eyelid lacerations: Prognosis is good. Generally heal without complication, unless the repair fails to realign the lid margin properly, this can result in failure of the eyelid to adequately distribute tear film and recurrent cornel ulceration..
- Bacterial and fungal ulcers: Have a favorable prognosis for retaining the eye and vision if they are recognized early and appropriate aggressive treatment is initiated.
- Conjunctival grafts and deep corneal ulcers: Prognosis is good to guarded. Often leave corneal scarring, even with successful treatment. This, however, does not appear to affect vision in most horses.
- Corneal perforation secondary to infection: Prognosis is guarded if immediate surgical intervention does not occur. In many horses, the globe will become blind and will shrink following rupture of a corneal ulcer, requiring removal of the eye (enucleation), if not promptly & aggressively treated.
- Corneal perforation associated with trauma: Prognosis is poor. Those associated with blunt trauma generally have a poorer prognosis than those caused by sharp trauma.
- Blunt trauma causes more bleeding and inflammation within the eye, and horses are more likely to have other damage to the inside of the eye.
- Short corneal lacerations (less than 15-mm) have a better prognosis for vision with repair than longer tears or those extending beyond the junction of the transparent cornea and sclera (white portion). Lacerations present for longer than two weeks or eyes that contain blood, infection, or other damaged tissues also have a poorer prognosis.
- Foreign body removal: Prognosis is generally good as long as the material has not penetrated the full depth of the cornea or other external structures of the eye.
- Fractures of the bony orbit: Carry a good prognosis for vision unless there is accompanying trauma to the eye. In these cases, the prognosis is dependent on the condition of the eye itself. There may also be cosmetic defects if there has been depression of the fracture fragments or bone loss.